COVID-19 increases value of oral appliance therapy for sleep apnea

Everyone knows that breathing is mandatory to sustain life, yet we rarely think about it, and often take it for granted! However, the current Flu Pandemic has certainly made us all too aware of its importance.
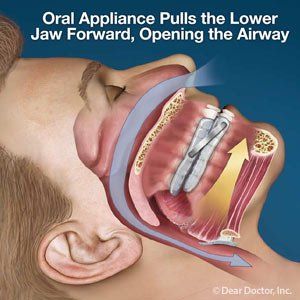
Obstructive Sleep Apnea (OSA) involves compromised breathing during sleep and is most often managed with Positive Airway Pressure (PAP). This device uses pressurized air to maintain airway patency during sleep. PAP has been considered “First Line” therapy for OSA since it was first introduced in the early 1980’s. Dentistry has an alternative to PAP for management of OSA, an Oral Appliance (OA), which maintains airway patency during sleep by holding the jaw in a forward position. Although PAP is considered “First Line” therapy for OSA, an OA is indicated as “Standard of Care” for all OSA severities if the patient cannot tolerate PAP, or if the patient simply prefers an OA to PAP. Studies demonstrate that only approximately 30-40% of patients wear their PAP all night, vs approximately 90% for OAs. Measurements of therapeutic benefit are similar for both devices, believed to be due to this much higher compliance rate. However, there is a very strong bias to prescribe PAP as Sleep Apnea therapy because PAP is more predictable at eliminating the OSA as measured by number of hourly events.
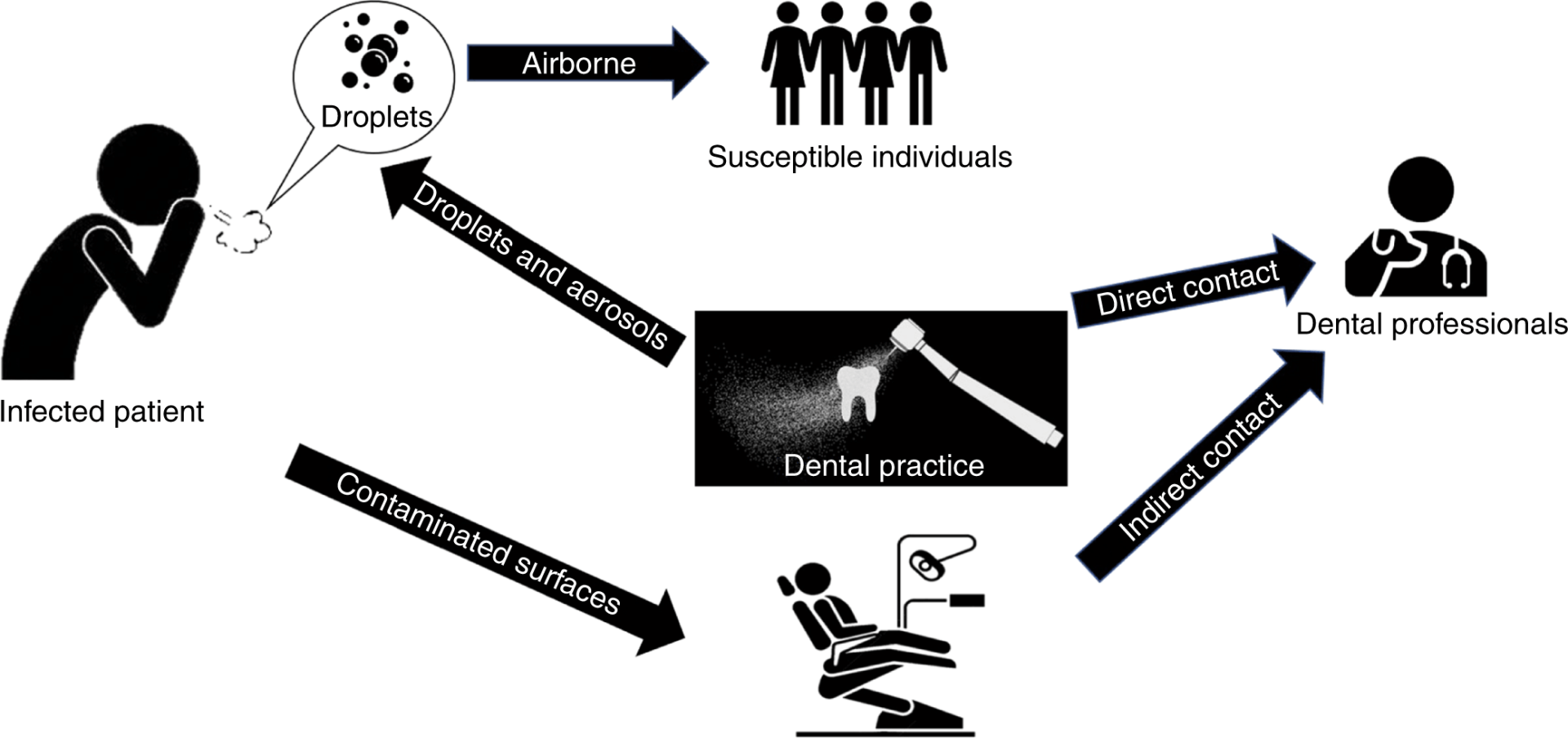
The COVID-19 Flu Pandemic has brought to light some very interesting concerns about use of Positive Airway Pressure (PAP) for the management of Obstructive Sleep Apnea (OSA). Although it has been known for some time that PAP can aerosolize respiratory droplets and spread them around the room during the night, it took the current Pandemic to highlight the medical implications associated with this; the potential to expose others to COVID-19. This is particularly concerning when one considers that OSA is estimated to afflict 1 Billion people globally, and for those that are managed, PAP is the most prevalent therapy.
PAP has been implicated with spreading COVID-19 within the Washington state nursing home that became ground zero in North America during this Pandemic. The First Responders that responded to the Life Care nursing facility in Kirkland Seattle late February used nebulizers and PAP machines to treat patients. “It’s best practice for us for people with respiratory illnesses,” said Jim Whitney, medical services administrator for the Redmond Fire Department. “We had no idea that we potentially had COVID patients there … We essentially aerosolized it,” said one responder after the fact, “We made it worse”. It was only later that King County public health officials advised Redmond Fire and other first responders in the region not to use PAP for patients suspected of having COVID-19 illness. Whitney said responders were using machines with specialized filters, which can reduce the amount of virus released. But King County public health authorities recommend that first responders avoid using PAP altogether. Redmond Fire has now discontinued the use of PAP for COVID-19 patients.
This March, the FDA published the following advisement, “If the number of ventilators in your facility is running low, consider alternative devices capable of delivering breaths or pressure support to satisfy medically necessary treatment practices for patients requiring such ventilatory support”, examples of alternative respiratory devices included PAP. They also recommended that appropriate precautions be exercised regarding environmental control or additional filtration where feasible, citing the concern for contamination of the room air and increasing risk of transmission. In April, Krieger and Thomas published an editorial in the Journal of Clinical Sleep Medicine which discussed that current PAP systems are “open” and do not filter expired air. They expressed concern of viruses being shed from the patients into the local environment. Using existing components, the authors described a circuit that they believe would be helpful in reducing viral shedding in COVID-19 patients on PAP devices. However, home PAP systems differ greatly by model and manufacturer and repurposing home units may be problematic. In spite of these efforts to make a PAP device more of a “closed” system, the fact remains that PAP is prone to leaks at the mask interface. In fact, ResMed, the inventor of PAP, provides the following perspective regarding mask leaks, a mask leak is not simply a “good vs. bad” dichotomy, but a spectrum, some degree of leak is quite acceptable. So, simply put, PAP masks will leak to some degree.
Out of concern for safety, there have been many other recommendations made regarding PAP use during this Flu Pandemic. The American Society of Anesthesiologists recently advised against PAP use for COVID-19 patients, this recommendation was based on experience with the SARS epidemic in 2003 along with studies that suggest PAP can pump viruses into the air, potentially increasing the spread of a contagious disease. Dr. Comilla Sasson, an associate clinical professor of emergency medicine at the University of Colorado School of Medicine recommends “not to use it … because we are concerned about community spread, and we have to assume that anybody with respiratory distress is a COVID-19 patient”. Toronto firefighters on overnight shifts are no longer allowed to personally use their PAP machines at work. Firefighters that use PAP during sleep will be moved to day shifts, and these measures will remain in effect until the COVID-19 risk has abated. This precaution is being taken to minimize the chance of spreading the virus, especially in light of the fact that some COVID-19 Positive patients are symptomless.
The American Academy of Sleep Medicine currently recommends that if a PAP user becomes positive for COVID-19, they should speak to their physician about assessing risks and benefits of continuing to use the PAP device at home. Persons at risk for infection from continued PAP usage include all cohabitants of the same household. In these cases, an Oral Appliance (OA) could be considered an effective alternative to PAP. An OA does not share any of the aerosol concerns associated with PAP use and is also much easier to disinfect daily in comparison to a PAP machine, hose and mask. For these reasons, the American Academy of Dental Sleep Medicine currently recommends that an OA should be prescribed as a First-Line therapy for OSA during the COVID-19 Pandemic.1 Of course, patients should not stop using their PAP without consulting with their physician first. If someone has tested positive for COVID-19 or presumes that they have some symptoms of the virus, then they should immediately sleep in separate rooms, and maintain distances even within the same household. They should also speak to their physician to help determine if they should continue PAP use. One needs to evaluate the pros and cons associated with spreading the virus all through the house vs. the specific individual’s circumstances and implications of not using it? Patients advised by their physician to stop using PAP should also avoid driving, because they may be sleep-deprived.
There has been much discussion about expecting a whole new “Normal” post COVID-19. Of course, a new level of vigilance will be exercised in the use of PPE once we are able to return to our offices. Likely, we will also be dealing with feelings of extreme apprehension from clinicians, team members and patients for the foreseeable future, this is human nature and unavoidable. Regarding OA therapy for management of OSA, it will be interesting to see if the well-entrenched bias for use of PAP over an OA to manage OSA will persist. I am anticipating that these current events will greatly influence the manner in which physicians, dentists, teams and patients view the OA alternative to manage OSA. Even the very best fitting PAP devices leak, this is simply a limitation of the technology, and acknowledged as acceptable by ResMed, the inventor of PAP. Now that we know about the liability associated with PAP, we can never unknow it! COVID-19 is not the first contagious virus, nor will it be the last.
References
-
Schwartz D, Addy N, Levine M, Smith H. Oral appliance therapy should be prescribed as a first-line therapy for OSA during the COVID-19 pandemic. J Dent Sleep Med. 2020;7(3)